Insuring the Integrity of Follicular Units
Let’s consider for a moment the other techniques that we think are integral to the follicular unit transplantation process. One is single strip harvesting, and the other is stereo-microscopic dissection. Without these companion techniques, the procedure may be called follicular unit transplantation, but it is a pale, inefficient imitation.
As its name implies, single strip harvesting is the method by which a single strip of hair-bearing scalp is carefully, indeed, painstakingly, excised from the donor area; the strip is then broken down into its smallest functional units, or follicular units. Before single strip harvesting came to the fore in recent years, older, infinitely more wasteful methods were employed. The first of these was the circular, punch grafts of yore, which have little to recommend them save their simplicity (they are essentially biopsy punches), and the ease with which they were directly placed into correspondingly circular holes in the recipient area. Next, ingenious surgeons devised multi-bladed scalpels; three or more (sometimes many more) blades, attached to a handle, were oriented parallel to one another, and many thin, narrow, long strips could be excised with one pass of the scalpel. These strips could then be placed flat on their sides and sliced into small mini- and micro-grafts, with little or no concern for follicular unit integrity. This, however, was not the only drawback; transection rates were generally rather high, and were even higher when more blades were used. So time was saved, but lots of valuable follicles were wasted.
What we know as single strip harvesting overcomes many of these disadvantages. Using a single blade with genuine open technique, it is possible, with experience and well training, the transection rates of several follicles is achieved. It is estimated that transection rates as high as 37% occur with the use of multi-bladed scalpels. Let’s do the math. If the patient needs 1000 grafts, then an area containing 1370 grafts would need to be removed just to account for wastage and still produce 1000 intact FU’s. If 2000 grafts were needed, 740 would need to be wasted! This is of serious import when we deal with a limited, finite amount of donor hair.
This leads us to a discussion of graft dissection. One of the reasons many surgeons have used multiple strip harvesting with multi-bladed scalpels, is that an intact, single strip presents a number of difficulties in dissection. It is too thick to place on its side or to shine light through (transilluminate) in order to visualize the individual FU’s. Therefore, thin, multiple strips lend themselves to rapid, albeit inefficient, slicing of grafts. We feel, however, that the degree of wastage is unacceptably high, both during the strip harvest, and during graft preparation.
Artistic Hairline Design
Hairline design is an important issue using combination of science and art. Proper hairline should be realistic, frame your face and match your age. Our doctor will discuss and ask your opinion to draw a new hairline which will be most suitable for your face. The creation of very small follicular unit grafts has enabled the hair surgeon to create very natural, feathered hairlines. Recently, we applied a portable laser device that can assist in symmetrical hairline placement in a few minutes.
Selection of safe permanent donor area
Safe Donor Zone from Unger Textbook
The permanent hair zone is selected and the hair is taped so after surgery the wound will be hided.
The selected hairs are shaved and the outline of strip is marked.
If you have ever seen a man with Class VII balding, and we all have, you have seen a graphic representation of the limits and confines of the donor area. This is the hair zone that is considered permanent. With rare exceptions, this rim of hair remains even in the most advanced cases of male pattern baldness. The boundaries of this zone extend from in front of the ears, around the temples, and to the back of the head. The hair at the temples may recede back toward the ear, and the balding area of the crown may dip quite low into the occipital area, at the back of the head. We must always assume that any man considering hair transplant surgery will eventually advance to this Class VII level for balding; it’s easy to understand why. Visible scars may be revealed if the baldness advances, and donor tissue has been taken too high, too low, or too far in front of the ears
Minimizing Donor Hair Wastage
We can directly measure not only the FU density, but the hair density as well, by using a tool called a densitometer or digital microscope (Proscope HR). With small areas of hair clipped short, a fixed area is observed under bright light and magnification. Then, we can calculate the appropriate numbers, for example: we can look at the density of FU’s and hair in the center of the back of the head, over the ear, and halfway in between. If the numbers average 1FU/mm2, and 2 hairs/FU, and the patient will be receiving 1500 grafts, then we can calculate that we will need to harvest about 15 square centimeters (cm2) from the back and side of the head to give us our required grafts. We can also assume that, given a 20% occurrence of single hair grafts in those with average density, our 20cm2 donor strip will provide us with about 300 single hair grafts, which should be enough for our hairline transition zone.
Moreover, we can use calculations to plan for the future. The average, non-balding person has about 100,000 hairs on the scalp. This would translate to 50,000 follicular units (FU’s). The “permanent zone” comprises about 25% of the total scalp; therefore, there would be one-fourth, or 25% of these total 50,000 FU’s in the permanent zone, which would equal 12,500 FU’s. We know that about half of the hairs in an area must be lost before there is any appearance of balding, so we could safely harvest up to half of the permanent zone FU’s, or 6,250 FU’s. This gives us an idea of the viable, reasonable donor reserves that a given patient has for current and future transplantation.
It is important to realize that the amount of coverage and density that a given person achieves with FU transplantation will vary not only according to their donor density and scalp laxity, but also according to their hair characteristics. This is another point where art meets science in the field of hair transplant surgery.
Anesthesia (Painless Hair Transplantation)
How we minimize discomfort of local anesthetic injection?
Buffering the Lidocaine by adding 7.5% sodium bicarbonate to Lidocaine neutralizes the acidic pH and decreases the pain of injection.
Warming the solution to body temperature lessens discomfort as well.
Cold compress with vibration before injection
We use smallest needle (30G) for infiltration
Slow injection
Hand holding, Talkanesthesia (talking while injecting) and Thai massage for pain distraction
Many people think of anesthesia as being “put to sleep”. However, there are other ways of achieving anesthesia, which just means rendering one insensitive to pain impulses. In hair transplantation we use local anesthesia, which, as the name implies, locally deadens (temporarily) the nerves, rather than the whole central nervous system (unconsciousness). This is most desirable because, when using local anesthesia, no pain is felt, the procedure can be done in the office, we avoid the expense and hazards of the hospital operating room and general anesthesia, and the patient is awake throughout the process, and can remain an active participant in decision making and respond to instruction from the physician during surgery.
There is better understanding of the relationship between effective anesthesia and limitation of bleeding or “oozing” during surgery. An inadequately anesthetized, anxious patient may have increases in heart rate and blood pressure that increase risk for bleeding; thus, anesthesia level and physical signs such as heart rate and blood pressure are carefully monitored during surgery.
Local anesthetics are injected into the skin and subcutaneous layers, and/or around larger nerves in the form of nerve blocks.
Nerve Blocks: infiltration of a small amount of anesthetic around a nerve trunk. It’s useful because it can substitute a single injection for a large number of injections and anesthetize a large area with a small amount of anesthetic.
Donor Area
Occipital nerve block, which is in the back of the head, above the neck. When this nerve is blocked, the back of the head (donor area) and crown are numbed; this can be of benefit after the surgery, also, as the donor area may be painful that night.
Donor Area Field Block
4 wheals are initially raised inferior to donor area by injecting anesthetic in the superficial dermis. A 30-gage needle (smallest as available) is then inserted dermally through the previously anesthetized wheal and the anesthetic is injected slightly to the right and then to the left until a solid line of anesthetic is created.
Recipient area anesthesia
Supraorbital nerve block
There is a pairs of nerve exit above the each eyebrows supply the frontal area of scalp. After this nerve block results in hairline and frontal area numbness. It’ll be pretreated with a topical anesthetic cream (5% EMLA) applied to the site of injection under occlusion for one hour combine with vibration will lessen the pain of the block. While waiting for the topical anesthetic to exert its effect, donor area anesthesia may be performed and the donor may be harvested.
Ring block
However, we do not do the surgery with just the blocks; we always inject locally, wherever incisions will be made. One of the reasons for this is that the blocks may be incomplete at times, and we want the scalp completely numb and unable to feel any pain. The other reason is to add epinephrine (adrenaline) to the area, this has a two-fold purpose: 1) to prolong and intensify the action of the local anesthetic and 2) to constrict the small blood vessels in the area and decrease the amount of bleeding. The importance of diminishing the amount of bleeding, especially in the recipient area, cannot be overemphasized. The less bleeding there is, the more easily and accurately the recipient incisions can be placed; likewise, with minimal bleeding, placement of the FU grafts causes less trauma to the follicles and is generally smoother and quicker.
Donor harvesting
Make sure every valuable follicle is not wasted.
Genuine Open technique donor harvesting
In 1997 Dr. Damkerng Pathomvanich was the first to develop and pioneer the OPEN TECHNIQUE in donor harvesting. This technique was published in the Dermatology Surgery Journal (April 2000) and Hair Forum International Journal (October 1998).
Because hair loss is on going processes, meaning that you have a limited donor hair to distribute to the area of balding scalp. Experienced and qualified hair surgeons are willing to spend more time in harvesting and cutting the grafts to achieve minimal wastage. Those who opt for quick blind techniques donor harvesting, will end up with significant follicular damage, up to 37% transection rate has been reported in medical literature. The damaged hair follicles usually have lower growth rate and, even if they do grow, they are deformed and miniaturized hair. This open method has one of the lowest transection rates when compared to other techniques reported in medical literatures. Minimal transection which means more grafts is available for transplantation and less skin has to be removed thus minimal donor scarring.
Prior incision, “tumescent” technique is applied this means is that a fairly large volume of fluid is injected into the numb donor area in order to raise the hair follicles up off the scalp; doing this allows us to cut more easily without damage to underlying nerves and blood vessels. In addition, when we free up the strip from its deeper tissues, we can do so with minimal damage to the bulbs of the follicles. Since the tumescent fluid is a saline solution with dilute amounts of local anesthetic and of epinephrine, the technique also helps to decrease bleeding and ensure that no pain is felt at any level of the dissection. After these injections various sensations like pulling or tightness may be felt, but there is no pain sensation.
After donor area is anesthetized and tumesced, the incision is scored superficially then pair of small double skin hooks are placed and gently pull in the opposite directions while cutting perpendicular using a single-bladed knife to between the hair follicles. In addition, 4 times magnification prismatic loupe and small tip suction is used to wipe out blood from the wound bed for better exposure. This enables individual hair follicles to be directly visualized and protected from transection during the painstaking harvesting process.
This technique is extremely efficient since it allows the surgeon to visualize the hair follicles before cutting, without needing to constantly guess the correct angle, while it requires more time and more experience; it provides an invaluable benefit to you. Higher and healthier grafts are obtained as a result.
When harvesting reach to 5-10 centimeters on both sides, the first piece of strip is removed for slivering and dissecting under stereo-microscope. The procedure is then carried out till the end of strip.
Graft Preparation: Slivering and Dissecting
The initial step of slivering the donor tissue into smaller units is the most crucial and technically exacting step. This use a single assistant who is very precise and capable of this step assures minimal transection of follicles. We apply a horizontal (coronal) slivering using x4 prismatic loupe or under 5-power magnifier with special designed plate give us faster and easier for further dissection.
To avoid unnecessary follicular transection, all graft production is accomplished under 10-power magnification binocular stereo-microscope and carefully trimmed into individual follicular unit graft then grouped separately into 1-hair, 2-hair, and 3-4 hair graft. Grafts are kept immersed in chilled holding normal saline solution at all the times.
We have a bacteriostatic humidifier running constantly during the surgery helps add moisture to the air and reduces graft drying.
Donor strip.
Piece of donor strip is slivered into thinner slices.
Slivers of donor strip.
Grafts are prepared under 10 times magnification stereo-microscope.
Graft dissection (small slivers are separated into each follicular unit).
1-4 hairs follicular unit grafts.
Each follicular unit is grouped and submersed in chilled normal saline ready to transplant.
Humidifier
Recipient Site Graft and Incisions
- Pre-made incision.
- Dense Packing.
- Tumescent fluid mixed with Triamcinolone acetate.
- Coronal Slit.
- Mega-session.
Pre-made incisions
After the donor site is closed, then the surgeon begins the tedious and painstaking process of creating the hundreds or thousands of recipient sites. These are generated using small needles or chisel-tip-micro-blade with depth control; the size of these miniscule incisions is based on several factors: the area of the scalp, the thickness and laxity of the scalp, and the size of grafts (one hair, two hair, etc) that will be placed. Great care is taken to avoid damage to existing hairs, and all this work is done under magnification (4x prismatic loupes as is the harvesting of the donor strip). This may be one stage of the surgery when talking to the surgeon is discouraged; it is necessary for us to keep count of hundreds or thousands of incisions being made. In this way, the number of grafts harvested will match up with the number of sites created.
Dense Packing
It is without question that, of all current graft types, follicular units can be placed into the smallest incisions; consequently, they can be placed in closer proximity in the scalp. Although it is not necessary to come close to the patient’s original density when transplanting, there is a certain minimum required to obtain coverage; also, the hairline especially needs closely, although somewhat randomly, placed single hair grafts to give the illusion of graded density.
Small incisions, moreover, simply heal more quickly than larger ones, and the grafts placed are less likely to suffer from blood-flow and oxygen deprivation. Any incision can damage the circulation of the scalp, causes scarring, and effect wound healing, hair growth, and even the potential for subsequent transplantation. In addition, small recipient sites, made with needles or micro blades, conserve the normal matrix structure of the scalp’s connective tissue. This allows the FU’s to fit snugly within the created sites, avoiding dislodgement, and promoting quicker healing and immediate nourishment of the grafts from local blood supply
Tumescent fluid mixed with Triamcinolone acetate
The tumescent technique that is used for the donor strip is also used to a degree in the recipient area. A saline solution, containing epinephrine and Triamcinolone acetate, is injected into the area, to “plump up” the scalp; this makes it less likely for the needles and mini-blades to lacerate blood vessels below the layer of the hair bulbs, and thus interfere with nourishment to the new grafts. And again, it decreases the amount of bleeding from the scalp, which greatly facilitates the creation of the recipient sites, and of the graft placement; this in turn may improve survival and growth of the FU grafts.
Triamcinolone acetate is a steroid adding to prevent post operative facial swelling especially at the eyelids and it does not interfere the survival rate of grafts.
Tumescent fluid is injected into the area, to “plump up” the scalp
The coronal slit (Perpendicular Angle Grafting or Lateral slit)
The coronal slit technique developed by Doctors Hasson and Wong is the only surgical method that is able to duplicate the alignment and distribution of hair as it occurs in nature, maximizing coverage, and eliminating the pluggy results of older hair transplantation methods. The angle and direction of hair growth can be precisely controlled, allowing transplantation of areas previously regarded as too difficult or unsuitable for hair transplant surgery, i.e. the temple and sideburn zones. In the donor area, follicular units appear to be lined up alongside one another in a plane perpendicular to the direction of hair growth. Lateral slit technique mimics nature’s arrangement of hair follicles providing the patient with the most natural possible results. In other methods of creating the recipient site, incisions are made sagitally, parallel to the direction of hair growth. In such methods, maximum possible density in a given area cannot be achieved, hairs grow randomly and often atop one another, producing redundant coverage and unnatural results.
Mega-Sessions (> 2000 grafts/session)
As it has become apparent that excellent growth can be realized with large FU sessions, other benefits have become manifest. For one thing, it advances the hair restoration process expediently. Most patients have no desire to get ensnared in a lengthy, repetitive series of treatments that they might even have to terminate prior to completion. A mega-session of FU’s, in some patients, can create a natural, undetectable result; this transplant can stand on its own, and continue to look natural even in the face of further hair loss, and without the necessary need for further work. In short, the process is just plain expedient and efficient.
Also, every time a procedure is done, the donor area is “violated”. One large, single strip harvested from the donor area will, by definition, create significantly less scarring, hair loss, and distortion of remaining hairs than will multiple, small strips, or, even worse, punch grafts. Minimizing the number of harvests, careful suturing and closure of the donor site, and close attention to harvesting technique can be invaluable in preserving precious donor resources; this is important not only in the event that further transplantation is desired, but also in preserving the cosmetic integrity of the donor area.
One other rationale for large sessions considers the need for different types of FU’s (i.e., singles, doubles, etc.). As we pointed out in the section on mathematical planning, only a certain percentage of FU’s will be single hair FU’s. This is quite important in planning the hairline reconstruction, which required relatively high numbers of singles. If too few FU’s are harvested, then the number of singles, for example, might fall short. In this case, the only options are an incomplete hairline, or “creating” singles by dividing 2 or 3 hair FU’s, which is definitely less than an ideal technique. Indeed, if we claim the primacy of the follicular unit, how can we then rationalize breaking them up?
Postoperative Care
Final check is done to make sure every graft properly positioned and elastic headband is placed at forehead to prevent facial swelling.
We generally use elastic headband with dressings cover the donor wound to keep hemostasis and forehead to prevent facial swelling. Patients will receive post-operative instructions at several stages of the treatment: often before, during and after the procedure, as well as in writing. Repetition of these guidelines is important for several reasons. Patients need to follow these directives carefully in order to insure the best possible growth of grafts and avoidance of complications. Also, people often forget what they are told within the context of the procedure, due to excitement, anxiety or information overload. Therefore, we try to reinforce the information at several points during the patient’s entire surgical experience.
What to expect after hair transplant surgery?
The night of the surgery, and for the next few nights afterwards, you are encouraged to sleep with your head elevated on pillows. You will be given medication to help you sleep if needed. The day after surgery, you come back and you will be taught and instructed how to shampoo and gently clean the transplanted area with a special shampoo, so after that you can take care yourself. The post-operative package will be given to you. The follicular unit grafts are made to fit snugly in the recipient site and will not be dislodged in the shower provided you follow the instruction given to you. After your first shower, 2 more days further head band are required.
If the post-operative instructions are followed carefully, in most patients the transplant is barely detectable after a few days and practically undetectable after the first week. Some patients experience swelling of the forehead that settles above the headband over the course of the next several days. If this occurs, put the headband back and it is almost always gone in the first week and should not be a cause for concern.
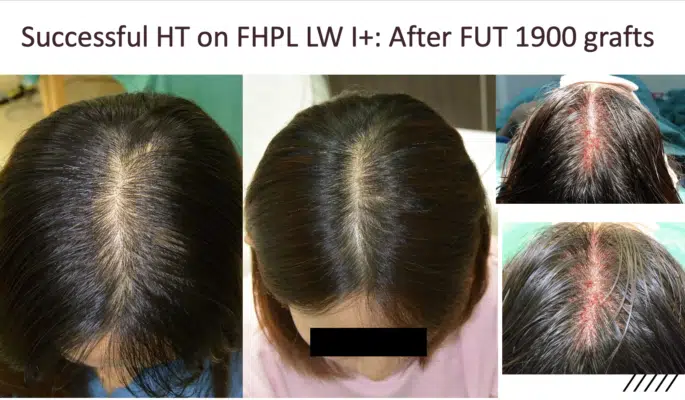
FUT result